9849193447
Know more about
Congenital Anophthalmia
Anophthalmia is a medical term that is used to describe the absence of the globe and ocular (eye) tissue from the orbit. The terms Anophthalmia and Microphthalmia(A/M) (small eyes) are often used interchangeably since CT scans or MRI show some remnants of either the globe or surrounding tissue in most cases. Anophthalmia/Microphthalmia (A/M) may affect one eye with the other eye being normal, or both eyes, resulting in blindness.
A/M is rare, but the exact incidence is unknown. One report from a prospective study of 50,000 newborns found an incidence of microphthalmia of 0.22 per 1,000 live births. In a recent study in England, the prevalence of anophthalmia and microphthalmia was 1.0 per 10,000 births.
A/M can be congenital (present at birth) or acquired later in life. A/M can occur alone or along with other birth defects. A/M may result from inherited genetic mutations, sporadic genetic mutations, chromosome abnormalities, prenatal environmental insult or other unknown factors.
Prevalence
True or primary anophthalmos is very rare. Only when there is complete absence of the ocular tissue within the orbit can the diagnosis of true anophthalmos be made. Extreme microphthalmos is seen more commonly. In this condition, a very small globe is present within the orbital soft tissue, which is not visible on initial examination.
There are three classifications for this condition:
Primary anophthalmia
is a complete absence of eye tissue due to a failure of the part of the brain that forms the eye.
Secondary anophthalmia
the eye starts to develop and for some reason stops, leaving the infant with only residual eye tissue or extremely small eyes which can only be seen under close examination.
Degenerative anophthalmia
the eye started to form and, for some reason, degenerated. One reason for this occurring could be a lack of blood supply to the eye.
Causes and Types & Treatments
Anophthalmia and microphthalmia may occur secondary to the arrest of development of the eye at various stages of growth of the optic vesicle. It is important to recognize microphthalmia because the development of the orbital region, as well as the lids and fornices, is dependent upon the presence of a normal-sized eye in utero. Anophthalmia is sometimes a clinical characteristic of Trisomy 13 (Patau syndrome) which is a Gross Chromosomal Abnormality.
TYPES: Consecutive anophthalmia, primary anophthalmia, and secondary anophthalmia.
Early treatment with various expanders or surgery, when necessary, will help decrease the orbital asymmetry and cosmetic deformities in these children.

Know more about
Anophthalmia

Know more about
Anophthalmic Socket
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
Acquired Anophthalmia
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
Phthisis Bulbi
A phthisis bulbi is a small, shrunken, non-functional eye. The affected eye may have partial vision retained in some cases; though blindness with this disorder is very common. The condition may result from an eye disease, trauma or inflammation. A phthisis bulbi, the eye has a scary and shrunken appearance. An eye ball may appear soft.
Alternative names: Phthisical globe
Causes & Risk factors
Phthisis bulbi occurs as a result of trauma, accident, exposure to the radiation, tumour, eye infection or inflammation.The severity of the disorder depends upon the type and depth of injury.
The injury or trauma can be a puncture wound, severe eye infection, inflammation within the eye itself etc.
The damage to structures within the eye from any of the above mentioned causes can eventually lead to eye atrophy i.e. shrinking.
Symptoms & Signs
The signs and symptoms of Phthisis bulbi are as listed as below:
Small and shrunken eye ball
Eye is in a distorted shape
Cornea may look scarred
Swelling in and around eye
Tender and painful eye
Early Cataracts
In case of an end-stage of phthisis bulbi, the retinal epithelium of the eye ball may undergo some bone formation. As a result the eye looks rough and bony.
Diagnosis
The doctor examines the eye carefully. He/she will also try to elicit the history of eye trauma, tumour, infection, injury and so on. As mentioned before, the Phthisis bulbi is always a response of the eye to some eye changes, leading to the eye damage.
Phthisis bulbi is characterized by a soft, shrunken eye. The presentation varies depending upon the severity and cause of the condition.
Biopsy of the affected eye: A histopathological study of a biopsy sample reveals the changes in the structure of an eye.
Computed Tomography (CT) scan: CT scan helps in studying the structural changes in the eye.
Prognosis
Prognosis of Phthisis bulbi is poor. The eye can become cancerous if left untreated.
Treatment Options
Medical:
If the patients suffer from loss of vision because of Phthisis bulbi; it cannot be corrected by any medical means. The treatment is directed towards the pain relief.
Pain relief: An injection of alcohol is given just behind the eye ball to relieve the pain.
Surgical:
Enucleation: It is a surgical procedure, in which the affected eye is removed from the socket, leaving behind rest of the orbital contents intact.
Differential Diagnosis
Tumours related to the eye like retinoblastoma, osteoma eye, oestrogenic sarcoma and uveal melanoma etc.
Blind eye, which is painful.
Age related calcific plaques.
Intraocular foreign implants.

Know more about
Painful Blind Eye
A painful, blind eye may result from any disease that causes blindness or a phthisical (shrunken, scarred, and non-functioning) eye. Acute causes include chemical or physical trauma, and chronic conditions include corneal decompensation and advanced and intractable glaucoma, especially neovascular glaucoma.

Know more about
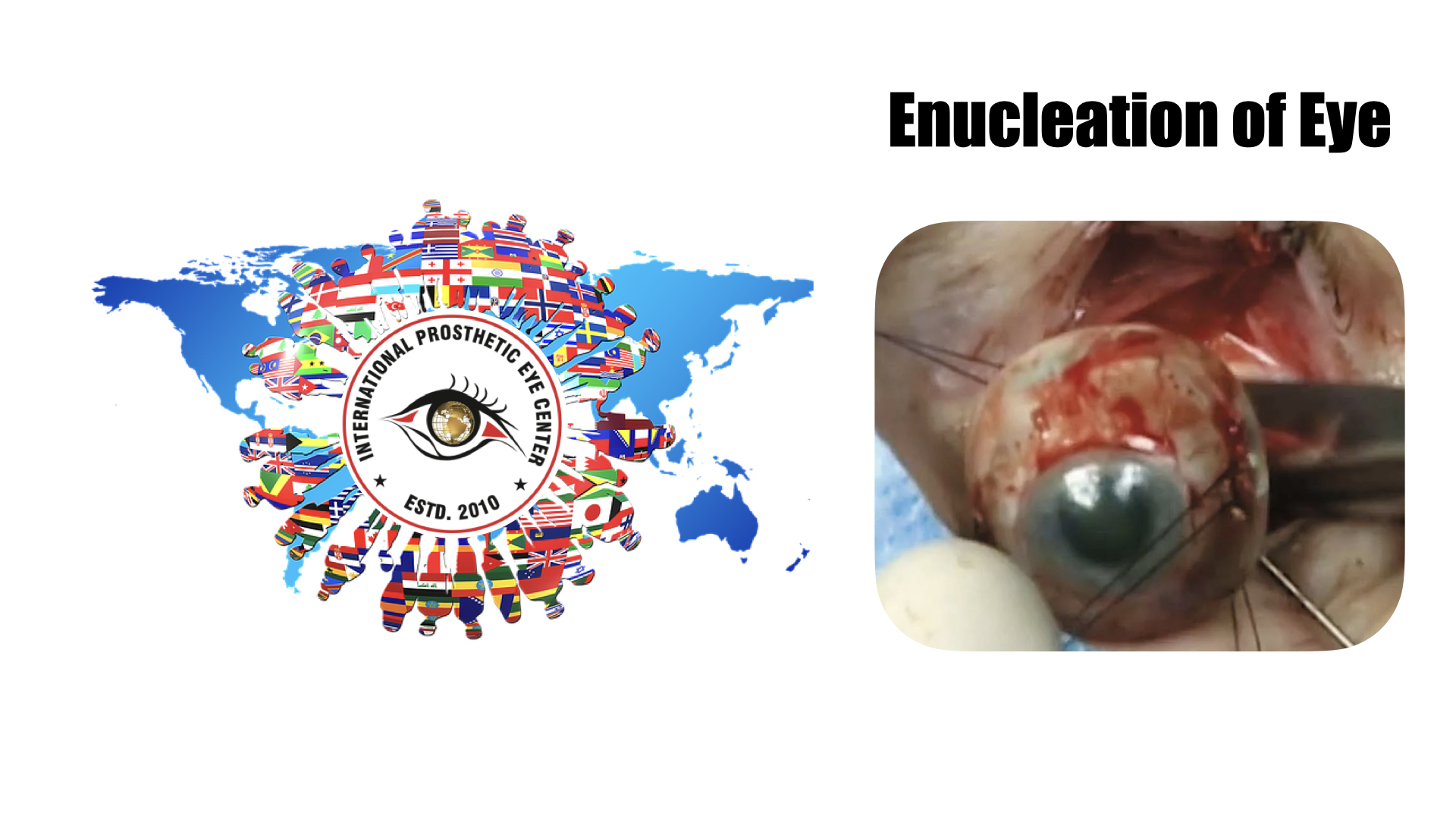
Enucleation of Eye
Enucleation is removal of the eye, leaving the eye muscles and remaining orbital contents intact. This type of ocular surgery is indicated for a number of different ocular tumors, in eyes that have suffered severe trauma, and in eyes that are blind and painful owing to other disease.[1]
Auto-enucleation (oedipism) and other forms of serious self inflicted eye injury are an extremely rare form of severe self-harm which usually results from serious mental illnesses such as schizophrenia.[2] The name comes from Oedipus, who gouged out his eyes in penance after having sex with his mother and killing his father.[3] Some patients have apparently been inspired by the Gospel of Matthew, which states: "...if the right eye offend thee, pluck it out and cast it from thee" (5:29).[4]
Classification
There are three types of eye removal
Evisceration - removal of the internal eye contents, but the sclera is left behind with the extraocular muscles still attached.
Enucleation - removal of the eyeball, but the adjacent structures of the eye socket and eyelids remain. An intraocular tumor excision requires an enucleation, not an evisceration.
Exenteration - removal of the contents of the eye socket (orbit) including the eyeball, fat, muscles and other adjacent structures of the eye. The eyelids may also be removed in cases of cutaneous cancers and unrelenting infection. Exenteration is sometimes done together with Maxillectomy which is removal of the maxilla or the upper jaw bone/cheekbone
Reasons for eye removal
Cancer of the eye (retinoblastoma, melanomas, any other cancers of the eye or orbit)
Severe injury of the eye when the eye cannot be saved or attempts to save the eye have failed
End stage glaucoma
Painful, blind eye
In cases of sympathetic ophthalmia (inflammation of the eye) to prevent travel to other eye, in which, if untreated can cause blindness
In a deceased person, so the cornea can be used for a living person who needs a corneal transplant by a surgical operation called keratoplasty.
Constant infection in a blind, or otherwise useless eye.
Know more about
Evisceration of Eye
An evisceration is the removal of the eye's contents, leaving the scleral shell and extraocular muscles intact.[1][2] The procedure is usually performed to reduce pain or improve cosmesis in a blind eye, as in cases of endophthalmitis unresponsive to antibiotics.[1][2] An ocular prosthetic can be fitted over the eviscerated eye in order to improve cosmesis.[3]
Either general or local anesthetics may be used during eviscerations, with antibiotics and anti-inflammatory agents injected intravenously.

Know more about
Acquired Anophthalmia
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
Socket contraction
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
Custom Conformer
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
Prolapse of socket
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
Post Eye Prosthesis
This is a block description. To edit, click and type the text or replace it with your own custom content

Know more about
NON-24
Non-24-hour sleep-wake disorder (N24) is a circadian rhythm sleep disorder in which an individual's biological clock fails to synchronize to a 24-hour day. Instead of sleeping at roughly the same time every day, someone with N24 will typically find their sleep time gradually delaying by minutes to hours every day.

Know more about
Custom Facial Prosthesis
The facial prosthesis is an artificial device used to replace a missing or malformed facial feature. Persons needing a prosthesis may have lost part of their face as a result of cancer, trauma or a congenital birth anomaly.
Know more about
Motion in eye prosthesis
This is a block description. To edit, click and type the text or replace it with your own custom content
Know more about
Auricular prosthesis
An auricular prosthesis is an artificial substitute for the auricle; the term epithesis is used synonymously. A myriad of materials have been used in the long history of anaplastology. However, the breakthrough came with the introduction of modern silicones and their colorings.